According to CMS, the top survey deficiency cited for hospice continues to be Standard §418.56(b)—Plan of Care. This regulation is fairly straight forward; however, state surveyors consistently find deficiencies. The issue often boils down to good communication between members of the interdisciplinary team (IDG) and adequate documentation. The IDG is responsible for collaborating with the…
According to CMS, the top survey deficiency cited for hospice continues to be Standard §418.56(b)—Plan of Care. This regulation is fairly straight forward; however, state surveyors consistently find deficiencies. The issue often boils down to good communication between members of the interdisciplinary team (IDG) and adequate documentation. The IDG is responsible for collaborating with the attending physician (if any), the patient or representative, and the primary caregiver to establish an individualized written plan of care. Problems identified during the initial, comprehensive, and updated comprehensive assessments, along with patient and family goals, must be addressed in the plan of care which is updated as needed during the course of care. The final requirement of this standard is education and training of the patient and primary caregiver(s) regarding care and services identified in the plan of care. It’s not uncommon for a member of the IDG to document a problem in the patient’s visit note but fail to update the plan of care with appropriate interventions and goals. A review of the patient’s plan of care and clinical record at least every 15 days should guide the team to determine the need for plan of care changes. Documentation of the review and any subsequent updates should keep the hospice in compliance with this standard.
-
 Hospice Survey Readiness Roadmap$150.00
Hospice Survey Readiness Roadmap$150.00 -
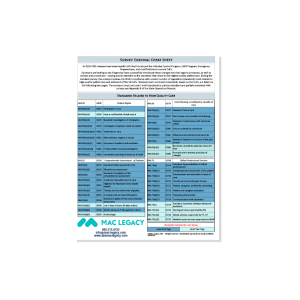 Survey Survival$45.00
Survey Survival$45.00 -
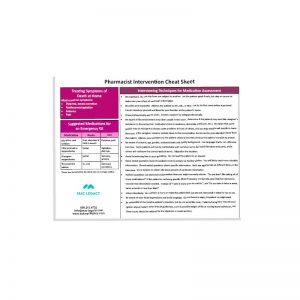 Pharmacological Interventions – Hospice$40.00
Pharmacological Interventions – Hospice$40.00 -
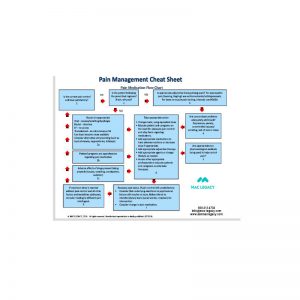 Pain Management Cheat Sheet$40.00
Pain Management Cheat Sheet$40.00 -
 Nutrition / Hydration / Nausea$40.00
Nutrition / Hydration / Nausea$40.00 -
 Delirium / Insomnia Cheat Sheet$35.00
Delirium / Insomnia Cheat Sheet$35.00 -
 Bowel Management Cheat Sheet$40.00
Bowel Management Cheat Sheet$40.00
